Severe anemia associated with intestinal bleeding
This is an online E-log book to discuss our patient's identified health data shared after taking his/ her guardians signed informed consent.
Here we discuss our individual patient problems through a series of inputs from available Global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
This E-log also reflects my patient centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
CASE SCENARIO:
A 32 year old female presented to the OPD with dysphagia, significant weight loss, pedal oedema, SOB on exertion, blood in stool and pain during defecation.
COMPLAINTS AND DURATION
Dysphagia to solids since 4 months (grade-3)
Weight loss of 15 kgs in 6 months
Pedal edema - relieved on medication outside hospital
Shortness of breath on exertion
Blood in stool , no malena
Pain during defecation
HISTORY OF PRESENT ILLNESS
Patient apparently asymptomatic , developed dysphagia which gradually progressed and the patient is now reluctant to take food.
HISTORY OF PAST ILLNESS
Not a K/C/O HTN, DM, asthma, epilepsy
Denovo detected hypothyroidism (started on 12.5 mg of thyronorm last month)
H/o hearing loss since childhood (not evaluated)
TREATMENT HISTORY
No significant treatment history
PERSONAL HISTORY
Single
Appetite - lost
Bowels- regular
Micturition -normal
No known allergies
No addictions
FAMILY HISTORY
No significant family history
MENSTRUAL HISTORY
Age of menarche - 14 years
Menstrual cycle = 28 days/ 3 days. Oligomenorrhea since 6 months.
PHYSICAL EXAMINATION
GENERAL
Weight - 34kgs
Pallor - Yes (severe)
Icterus - No
Cyanosis - No
Clubbing of finger/toes - No
Lymphadenopathy - No
Oedema - yes
Malnutrition - yes
Dehydration - yes
Koilonychia - present
Grade 1 goitre
Temperature - afebrile
Pulse rate 54 b/min
Respiration rate - 17/min
BP 80/60 mmHg
SYSTEMIC EXAMINATION
CARDIOVASCULAR SYSTEM
Thrills - No
Cardiac sounds - S1 , S2 positive
RESPIRATORY SYSTEM
Dysponea - No
Wheeze - No
Position of trachea - Central
Breath sounds - Vesicular
Adventitious - Rhonchi
ABDOMEN
Shape of abdomen - Scaphoid
CENTRAL NERVOUS SYSTEM
Level of consciousness
Alert
Stuporous
Signs of meningeal irritation
Neck stiffness - no
Kerning’s sign - no
Cranial nerves - normal
Motor system - normal
Sensory system - normal
Glasgow system - normal
Cerebral signs
Finger nose coordination - Yes
Knee Heel In-coordination - Yes
F.MUSCULO SKELETAL SYSTEM - normal
G. SKIN - normal
H. EXAMINATION OF BREAST - normal
I. EXAMINATION OF ENT - normal
J.EXAMINATION OF TEETH AND ORAL CAVITY - normal
K. EXAMINATION OF HEAD AND NECK - normal
PROVISIONAL DIAGNOSIS/ DIAGNOSIS
Severe anaemia (? Iron deficiency anemia) 2 nd degree to
Blood loss ( H/o Haemorrhoids)
Nutritional cause
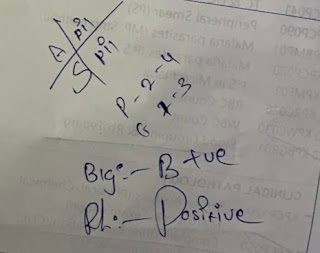
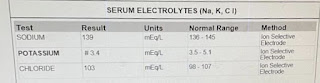
HAEMOGRAMBLOOD UREABLOOD GROUPING AND RH TYPINGECGSERUM CREATININELFTSERUM ELECTROLYTESHIV TESTHEPATITIS C TESTHEPATITIS B TEST










Comments
Post a Comment